This article accompanies a prototype NHS booking system for GP appointments, which explores alternative models for primary care access. Note: This is an exploratory concept designed to contribute to discussion around NHS service access and digital infrastructure. Source code available here.
The current GP model in the UK features structural barriers that can prevent patients from accessing care when and where they need it.
GP practices are commissioned by the NHS but operate with a high degree of independence, including how they procure and manage clinical software. Each practice typically licences its own appointment system, triage platform, and patient record system—leading to a patchwork of different technologies that often don’t work well together. When patients relocate, travel, or access care outside their home area, their records may not follow. This creates friction in care continuity, administrative complexity, and inconsistent access to patient history.
A Costly Patchwork
From an NHS perspective, this decentralised procurement model adds hidden costs. Licensing fees and integration contracts across hundreds of individual practices inflates IT spending. Data loss during system migrations, such as missing clinical notes or allergy history, further undermines care quality and poses clinical safety risks when essential history is missing or obscured.
The funding structure for GP practices also contributes to these challenges. The current capitation model (payment per registered patient) incentivises practices to limit access to registered patients only. This approach may prevent efficient allocation of resources across the NHS, contributing to postcode-based disparities in care.
Furthermore, patients are often encountering a Locum or Healthcare Assistant instead of the ‘Family Doctor’, lengthy waits for routine appointments whilst nearby practices may have availability, and complex bureaucracy when needing care away from home.
Open Access Vision
This system proposes a transformation: all NHS primary care providers—GP surgeries, walk-in centres, urgent care clinics, and community health hubs—should be treated as part of a single, open-access network of care.
Patients should be able to book appointments at any of these locations, just as they can attend any NHS A&E department in a crisis.
A patient’s NHS Login or GOV.UK One Login would become their primary identifier, replacing registration at a home practice, and allowing records to follow them across all facilities.
Rethinking the Funding Model
By tracking patient access across healthcare locations, practices could be reimbursed per consultation or outcome, rather than block funding based on patient lists. This model incentivises practices to provide excellent care to attract patients and would allow commissioners to distribute resources based on real demand patterns.
Crucially, it could reduce duplication of systems and licenses. Instead of every practice procuring its own appointment and records software, Open Access Booking could offer a unified interface with a national open standard underneath. This reduces IT spend while improving consistency and encouraging responsiveness and equality of access—particularly in underserved areas.
Unified Booking Platform
The envisioned system offers a single digital front door for all NHS primary care. Patients would see real-time availability across all nearby NHS services. The system would route bookings based on urgency, location, and capacity, and integrate with existing NHS App infrastructure.
A Prototype Towards Reform
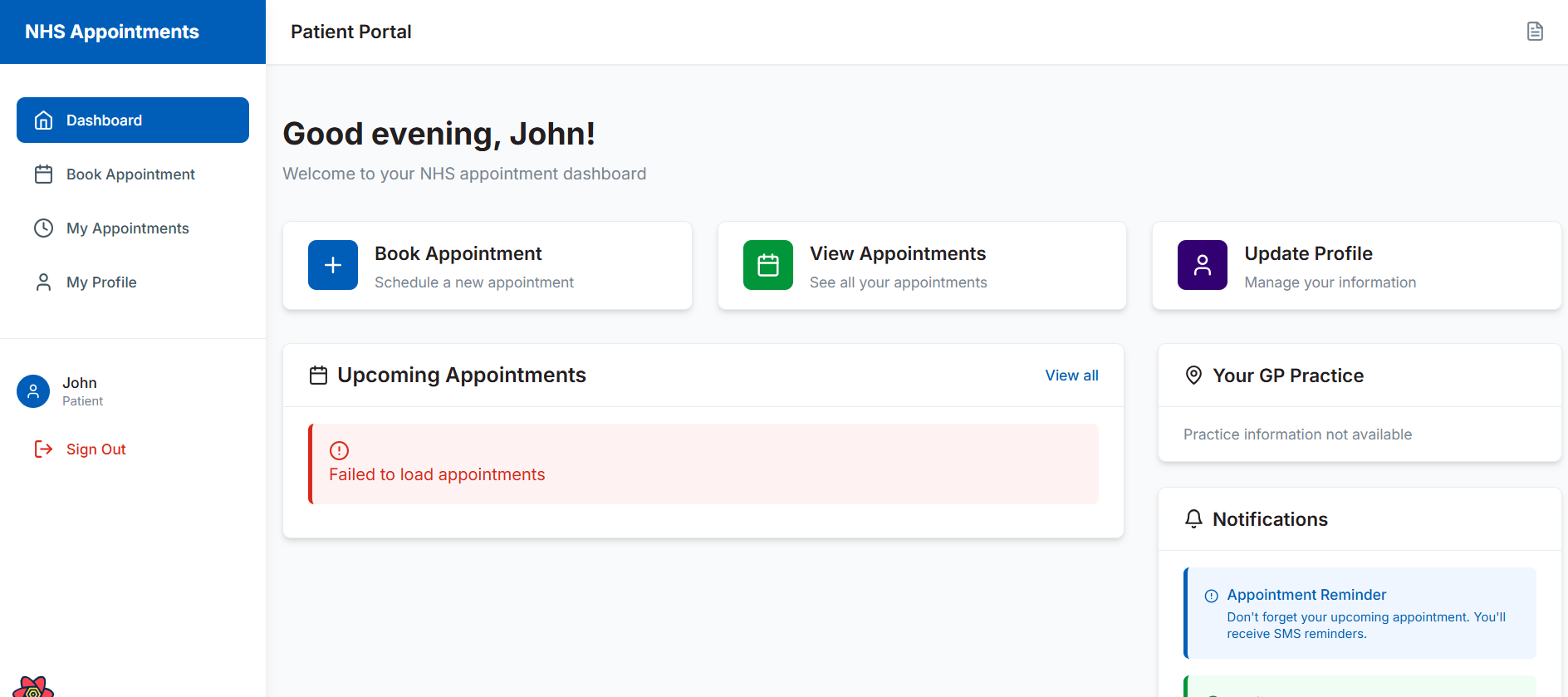
This appointment booking system prototype offers a vision for how things could work differently. Instead of having various fragmented booking systems between practices, this platform is built to function across organisational boundaries. Rather than require every patient to register with a single practice to receive care, it treats all clinics, walk-in centres, and GP surgeries as open-access NHS services.
This is not to remove the role of the family doctor, but rather to provide a flexible alternative when continuity isn’t possible—ensuring patients can still access timely, safe care wherever they are. Using a common appointment object and federated patient identity (via NHS Login or GOV.UK One Login), the app enables patients to book care at multiple locations, with confidence their data can travel too.
A deeper dive
In this prototype, the backend is built using serverless architecture (AWS Lambda and DynamoDB) for cost-effectiveness. Identity is handled with NHS-compatible JWTs, while patient and practice data structures are FHIR-aligned and future-proofed for integration with NHS Spine and GP Connect.
For now, the prototype uses a dual-storage model: capturing human-readable medical data alongside placeholders for SNOMED CT and dm+d codes. This allows the system to function with test data or pilot users, while remaining ready for full NHS alignment when access to clinical coding APIs and sandbox environments becomes available..
Final Remarks
This app is not integrated with NHS systems or approved for clinical use. But it is a demonstration of what’s possible with modern tooling, thoughtful design, and a commitment to cohesive tech. It imagines a future where practices can focus on delivery rather than bureaucracy.
By building openly and with standards in mind, we invite others—developers, clinicians, commissioners—to consider what primary care could look like if we aimed to minimise technical fragmentation and consider more flexible approaches.
Leave a Reply